 |
| Von Willebrand disease by Pharmacytimess |
Overview
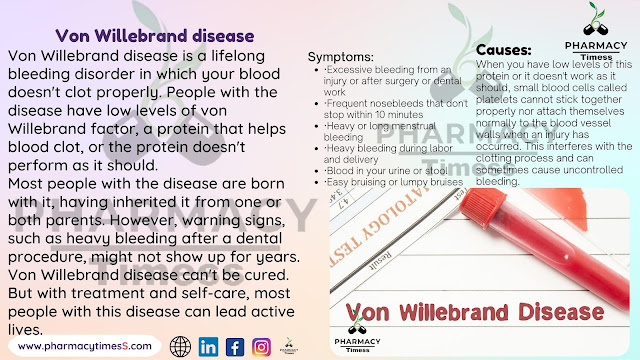
Von Willebrand disease is a lifelong bleeding
disorder in which your blood doesn't clot properly. People with the disease
have low levels of von Willebrand factor, a protein that helps blood clot, or
the protein doesn't perform as it should.
Most people with the disease are born with it,
having inherited it from one or both parents. However, warning signs, such as
heavy bleeding after a dental procedure, might not show up for years.
Von Willebrand disease can't be cured. But
with treatment and self-care, most people with this disease can lead active
lives.
Symptoms
Many people with von Willebrand disease don't
know it because the signs are mild or absent. The most common sign of the
condition is abnormal bleeding.
There are three main types of the disease. The
amount of bleeding varies from one person to another, depending on the type and
severity of the disease.
If you have von Willebrand disease, you might
have:
·
Excessive bleeding
from an injury or after surgery or dental work
·
Frequent nosebleeds
that don't stop within 10 minutes
·
Heavy or long
menstrual bleeding
·
Heavy bleeding during
labor and delivery
·
Blood in your urine or
stool
·
Easy bruising or lumpy
bruises
Menstrual signs and symptoms might include:
·
Blood clots greater
than 1 inch (2.5 centimeters) in diameter in your menstrual flow
·
The need to change
your menstrual pad or tampon more than once an hour
·
The need to use double
sanitary protection for menstrual flow
·
Symptoms of anemia,
including tiredness, fatigue or shortness of breath
When to see a doctor
Contact your doctor if you have bleeding that
lasts a long time or is hard to stop.
Causes
The usual cause of von Willebrand disease is
an inherited abnormal gene that controls von Willebrand factor — a protein that
plays a key role in blood clotting.
When you have low levels of this protein or it
doesn't work as it should, small blood cells called platelets cannot stick
together properly nor attach themselves normally to the blood vessel walls when
an injury has occurred. This interferes with the clotting process and can
sometimes cause uncontrolled bleeding.
Many people with von Willebrand disease also
have low levels of factor VIII, another protein that helps in clotting.
Factor VIII is involved in another inherited
clotting disorder called hemophilia. But unlike hemophilia, which mainly
affects males, von Willebrand disease affects males and females and is usually
milder.
Rarely, von Willebrand disease can develop
later in life in people who didn't inherit an affected gene from a parent. This
is known as acquired von Willebrand syndrome, and it's likely caused by an
underlying medical condition.
Risk factors
The main risk factor for von Willebranddisease is having a family history of it. Parents pass the gene for the disease
to their children. Rarely, the disease skips generations.
The disease is usually an "autosomal
dominant inherited" disorder, which means you need a mutated gene from
only one parent to get the disease. If you have the gene for von Willebrand
disease, you have a 50% chance of transmitting this gene to your children.
The most severe form of the condition is
"autosomal recessive," which means both of your parents have to pass
a mutated gene to you.
Complications
Rarely, von Willebrand disease can cause
uncontrollable bleeding, which can be life-threatening. Other complications of
von Willebrand disease can include:
·
Anemia. Heavy menstrual bleeding can cause iron
deficiency anemia.
·
Swelling
and pain. This can be a
result of abnormal bleeding in the joints or soft tissue.
Prevention
If you plan to have children and have a family
history of von Willebrand disease, consider genetic counseling. If you carry
the gene for von Willebrand disease, you can pass it on to your offspring, even
if you don't have symptoms.
Diagnosis
Mild forms of von Willebrand disease can be
difficult to diagnose because bleeding is common, and, for most people, doesn't
indicate a disease. However, if your doctor suspects you have a bleeding
disorder, he or she might refer you to a blood disorders specialist
(hematologist).
To evaluate you for von Willebrand disease,
your doctor will likely ask you detailed questions about your medical history
and check for bruises or other signs of recent bleeding.
Your doctor will also likely recommend the
following blood tests:
·
Von
Willebrand factor antigen. This
determines the level of von Willebrand factor in your blood by measuring a
particular protein.
·
Von
Willebrand factor activity. There
are a variety of tests to measure how well the von Willebrand factor works in
your clotting process.
·
Factor
VIII clotting activity. This
shows whether you have abnormally low levels and activity of factor VIII.
·
Von
Willebrand factor multimers. This evaluates the structure of von Willebrand factor in
your blood, its protein complexes and how its molecules break down. This
information helps identify the type of von Willebrand disease you have.
The results of these tests can fluctuate in
the same person over time due to factors such as stress, exercise, infection,
pregnancy and medications. So you might need to repeat some tests.
If you have von Willebrand disease, your
doctor might suggest that family members undergo tests to determine if this
condition runs in your family.
Treatment
Even though von Willebrand disease has no
cure, treatment can help prevent or stop bleeding episodes. Your treatment
depends on:
·
The type and severity
of your condition
·
How you've responded
to previous therapy
·
Your other medications
and conditions
Your doctor might suggest one or more of the
following treatments to increase your von Willebrand factor, strengthen blood
clots or control heavy menstrual bleeding:
·
Desmopressin. This medication is available as an
injection (DDAVP). It's a synthetic hormone that controls bleeding by
stimulating your body to release more of the von Willebrand factor stored in
the lining of your blood vessels.
Many doctors consider DDAVP the first treatment for
managing von Willebrand disease. It can be used before minor surgical
procedures to help control bleeding. You might be given a trial of desmopressin
to make sure it's effective for you.
·
Replacement
therapies. These include
infusions of concentrated blood-clotting factors containing von Willebrand
factor and factor VIII. Your doctor might recommend them
if DDAVP isn't an option for you or has been ineffective.
Another replacement therapy approved by the Food and Drug
Administration for treating adults 18 and older is a genetically engineered
(recombinant) von Willebrand factor product. Because recombinant factor is made
without plasma, it can reduce the risk of a viral infection or allergic
reaction.
·
Oral
contraceptives. In addition to
preventing pregnancy, these drugs can help control heavy bleeding during
menstrual periods. The estrogen hormones in birth control pills can boost von
Willebrand factor and factor VIII activity.
·
Clot-stabilizing
medications. These
anti-fibrinolytic medications — such as aminocaproic acid (Amicar) and
tranexamic acid (Cyklokapron, Lysteda) — can help stop bleeding by slowing the
breakdown of blood clots. Doctors often prescribe these drugs before or after a
surgical procedure or tooth extraction.
·
Drugs
applied to cuts. A fibrin sealant
(Tisseel) placed on a cut helps curtail bleeding. This is applied like glue
using a syringe. There are also over-the-counter products to stop nosebleeds.
If your condition is mild, your doctor might
recommend treatment only when you're having surgery or dental work or when
you've had a trauma, such as a car accident.
Lifestyle and home
remedies
These self-care tips can help you manage your
condition:
·
Switch
pain relievers. To help prevent
bleeding episodes, talk with your doctor before taking blood-thinning
medications — such as aspirin, ibuprofen (Advil, Motrin IB, others) or naproxen
sodium (Aleve). Your doctor might instead recommend pain and fever relievers
such as acetaminophen (Tylenol, others).
·
Tell
your doctors and dentist. Let
your doctors or dentist know that you have von Willebrand disease before you
have surgery, start a new medication or give birth. Also mention whether anyone
in your family has a history of excessive bleeding.
·
Consider
wearing a medical ID bracelet. Make sure it notes that you have von Willebrand disease,
which will be helpful to medical personnel if you're in an accident or taken to
an emergency room. Also carry a medical alert card in your wallet.
·
Be
active and safe. Exercise is part
of attaining or maintaining a healthy weight. Avoid activities that could cause
bruising, such as football, wrestling and hockey.
Preparing for your
appointment
You'll likely see your family doctor if you
think you have a bleeding problem. You then might be referred to a doctor who
specializes in the diagnosis and treatment of bleeding disorders
(hematologist).
Here's some information to help you get ready
for your appointment.
What you can do
Ask about pre-appointment restrictions when
you make the appointment. You might need to follow dietary restrictions or fast
for 8-10 hours if blood tests are scheduled.
Make a list of:
·
Signs
or symptoms that involve bleeding, including how often, how severe and for how long. Include
unusual bruising. Your doctor will want to know if you have a history of
nosebleeds or easy bruising since childhood. If you menstruate, are your
periods extended and heavy?
·
Key
personal information, including major
stresses or recent changes — both positive and negative.
·
Key
medical information, including other
medical problems and close relatives who bleed easily. Also list medications,
vitamins or other supplements you take, including doses.
·
Questions
to ask your doctor.
Take a family member or friend along, if
possible, to help you remember the information you'll be given.
For von Willebrand disease, questions to ask
your doctor include:
·
What's the most likely
reason for my symptoms?
·
What treatment do you
recommend, and how will you monitor whether it's working?
·
What are the possible
side effects of the medications you're prescribing?
·
Does this condition
increase my risk of other medical problems?
·
What will I need to do
before having surgery or dental procedures?
·
Does this condition
increase my risk of health problems during pregnancy and childbirth? Are
treatment options available to reduce that risk?
·
Do I need to avoid
certain physical activities or types of exercise?
·
I have other health
conditions. How can I best manage them together?
What to expect from
your doctor
Your doctor might ask:
·
Have you had bleeding
from a small wound that lasted more than 15 minutes or recurred during the week
following the wound?
·
Have you had a
nosebleed that lasted more than 10 minutes or needed medical attention?
·
Have you had
unexpected bruising? Have you ever felt a lump under the bruise?
·
If you menstruate, how
many days do your periods last? How often do you change your tampon or sanitary
pad during a period? Have you seen blood clots in your menstrual flow?
·
Have you had blood in
your stool that wasn't explained by a known medical problem, such as a stomach
ulcer or colon polyp?
·
Have you ever needed
medical attention for bleeding during or after surgery, dental procedures,
childbirth or injury?
·
Have you had anemia or
needed a blood transfusion?
What you can do in the
meantime
While you wait for your appointment, avoid
pain relievers that can increase your risk of bleeding, such as aspirin,
ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). If you need
relief for aches and pains, try acetaminophen (Tylenol, others) instead.
Steer clear of contact sports associated with
a high risk of bruising or injury, such as football and hockey. If you have
medical or dental procedures scheduled, tell your doctor or dentist about your
history of heavy bleeding from minor injuries.
If you're having a procedure that's not
urgent, reschedule it until after you've been evaluated for a bleeding
disorder.





0 Comments